|
Case Report
Osteochondromatosis of the shoulder with massive rotator cuff tear and marked degenerative arthropathy: A case report
1 Department of Radiology, Ibn Sina Hospital, Rabat, Morocco
Address correspondence to:
Arthur Semedo Insumbo
Department of Radiology, Ibn Sina Hospital, Rabat,
Morocco
Message to Corresponding Author
Article ID: 100015R02AI2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Insumbo AS, Bizimana W, Jroundi FL, Laamrani FZ. Osteochondromatosis of the shoulder with massive rotator cuff tear and marked degenerative arthropathy: About a case with review of literature. Edorium J Radiol 2020;6:100015R02AI2020.ABSTRACT
Synovial osteochondromatosis (SO) is a benign monoarticular disorder of unknown origin that is characterized by synovial metaplasia and proliferation resulting in multiple intra-articular cartilaginous loose bodies of relatively similar size, not all of which are ossified. It has been considered a rare condition with a frequent tendency to occur in the hips, elbow, and shoulder. Usually, the condition is monoarticular affecting any joint but the large joints are preferentially affected: knee (up to 65%), hips (25%). Occasionally, bursa or tendon sheaths may be involved. We report a case of osteochondromatosis with a rare localization, diagnosed through magnetic resonance imaging (MRI).
Keywords: Massive rotator cuff tears, Osteochondromatosis of the shoulder
INTRODUCTION
Synovial osteochondromatosis (SO) has been characterized by authors as being osteoarticular anomaly that develops preferentially in the synovium of joints, bursa, and tendon sheaths, with particular tendency for young people and adults. It is in fact a relatively rare condition, the shoulder being less affected compared to elbow and hips, where it has a reported incidence of 1.9–5.2% of all sites [1],[2],[3],[4],[5].
Synovial osteochondromatosis is classified into two types: primary and secondary types. Primary SO is extremely uncommon [2],[3],[4]. The images that appear on MRI are always variable depending on the relative preponderance of the proliferation of synovial cartilages formation size of loose bodies, the extent of the ossification and the extent of decalcification.
The therapy for SO of the shoulder over the years is generally the same, although there have been enormous technical developments. Arthroscopic treatment is the gold standard for the resection of intra-articular foreign bodies. Synovectomy and partial or total capsulotomy may not be systemic depending on the radiological assessment made at the MRI as during surgical intervention [3].
Magnetic resonance imaging shows unmineralized nodules that demonstrate typical chondroid signal characteristics:
T1: intermediate to low signal, and
T2: high signal
In some cases focal areas of signal void can be seen within these nodules representing areas of mineralization [5].
We report a case of chondromatosis in an elderly patient with chronic pain with no other known antecedents. For the publication of this clinical case, the patient was informed that her data would be submitted for publication, and provided the appropriate consent.
CASE REPORT
An 85-year-old female, 1.54 meters tall and weighing 76 kg, farmer, with no pathological history, developed left shoulder pain over three years without any known precipitating factor. She presented to our department because of increasing pain and gradual difficulty in raising her left arm. Physical examination on presentation did not reveal any swelling or feeling of heat in the left shoulder. A complete blood count was normal.
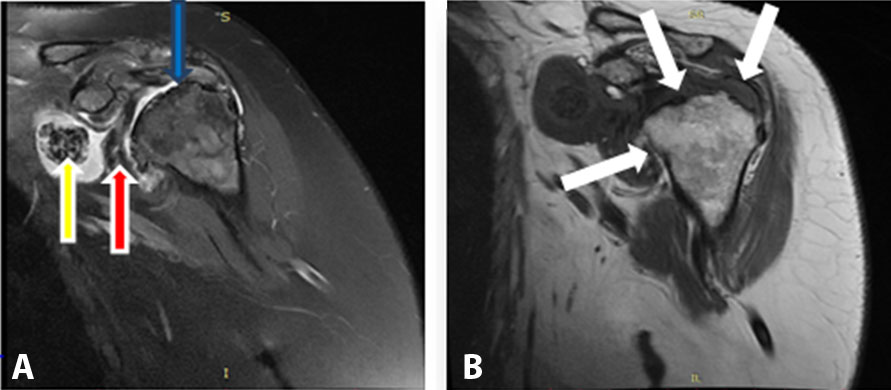
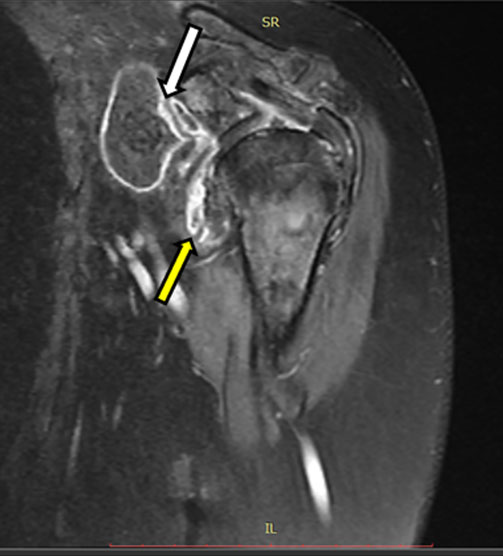
A plain MRI of the shoulder showed: unmineralized nodules that demonstrated typical chondroid signal characteristics: T1a coronal proton density MRI: intermediate to low signal and T2: high signal (Figure 1), Irregularity of the humeral head (yellow and red arrow) with presence of intra-articular foreign bodies (blue arrow), T1b: Arthroses (white arrow).
In T1 with injection: thickening of the synovium that was raised after gadolinium injection around recesses around foreign body (Figure 2). Gradient echo (GE): showed blooming artifact.
After the clinical examinations and radiological observation, our patient was finally diagnosed with synovial osteochondromatosis of shoulder associated with shoulder arthropathic changes. The treatment was based on surgical resection, removing the foreign body completely without incident, which allowed the patient to return to clinical normalization.
DISCUSSION
Synovial osteochondromatosis can affect any synovial cavity. It is an uncommon condition, most often seen in men between the third and fifth decades. It is usually monoarticular, most frequently affecting the knee and hip joints [5]. The incidence of osteochondromatosis affecting the shoulder is unclear, but it is certainly rare. In three reported case series of SO involving almost 110 patients, the shoulder was affected in only seven patients [3],[4],[5].
Synovial osteochondromatosis can be considered either primary (idiopathic) or secondary, occurring as a sequel of intra-articular pathology, such as a traumatic osteochondral defect [6]. Subsequent enlargement results from proliferation of connective tissue cells and cartilaginous metaplasia, and the characteristic loose bodies develop [7],[8].
In our case the presence of arthroses suggests a secondary disease with a history of prolonged symptoms.
It is considered to fall under the umbrella of non-septic articular disorders, and symptoms are often non-specific, the clinical signs of pain, swelling, and reduced range of movement overlap with many other disorders [1].
Lunn et al. [9] reported 18 patients with SO. All of them presented with pain and loss of function. Although locking and instability are commonly reported as a result of intra-articular loose bodies, only six patients in this series reported such symptoms [9].
Diagnosis of SO is usually made from the pathognomonic plain radiography features. Multiple intra-articular calcifications of a similar size and shape are distributed throughout the joint[3]. Radiological examination such as computed tomography (CT) and MRI optimally demonstrate bone or articular surface erosion and synovial involvement, although osteochondromatosis can be reliably diagnosed by plain radiography in 70–90% of cases[3],[10],[11]. Surgical excision of the loose bodies and synovectomy is the usual treatmentt [9].
Radiological findings depend on the form of the disease (primary or secondary), their stage and the presence of calcification or ossification of the cartilaginous nodules [1],[12].
In primary osteochondromatosis, the study by radiography can identify increased joint space and volume increase of the periarticular soft tissues associated with erosions of the articular margins, indicating the presence of intra-articular disease [10]. Calcifications are often numerous, sometimes uncountable, and similar in size and format. Generally they are of the ring type of the cartilaginous origin. Common periarticular osteoporosis is not found.
In the secondary form of the disease we find signs of degenerative joint disease (reduction of articular space, marginal osteophytes, sclerosis and subchondral bone cysts), associated with a smaller number of calcifications, which present varying sizes, usually larger, and calcify more irregularly or in concentric layers. This last description is almost similar to that found in our patient.
On ultrasonography the cartilaginous nodules present a hypoechogenic aspect, and calcifications increase their echogenicity, being able to determine posterior acoustic shadow.
In the shoulder, the ultrasound has a particular sensitivity for the detection of the disease affecting the sheath of the tendon of the biceps long head while demonstrating nodules adhered to the synovial surface, which is usually found facilitated by the presence of fluid inside the synovial sheath. Free bodies are often found along the bicipital groove [9],[12],[13]. These patients often have secondary form of the disease, associated with other alterations found in the shoulder exam, such as joint and subacromial-deltoid bursa, tendinopathies, and tendinous ruptures.
The images that appear on MRI are always variable depending on the relative preponderance of the proliferation of synovial cartilages, formation in quantity and size of loose bodies, on the other hand, the extent of the ossification and the existence or not of decalcification must be considered [12].
Non-calcified lesions form a synovial thickening or an intra-articular mass iso-intense to the muscle in the T1-weighted, and hyper-intense in the T2-weighted sequences [1],[12],[14].
These lesions may be differentiated from joint effusion or other soft tissue tumors by the presence of characteristic impregnation of chondral lesions with peripheral pattern and septal levels after gadolinium-based intravenous contrast[1],[13]. Contrast also assists in the detection of inflammatory activity of the disease by the presence of synovial impregnation. Calcified nodules have low signal in all sequences used.
Intra-articular nodules undergoing ossification are composed of mature bone, have a cortical bone in the periphery with low signal intensity, and bone marrow hyperintense inside the T1-weighted sequences.
This case illustrates the diagnosis of secondary SO in a patient who presented with shoulder pain and loss of function.
Clinicians should maintain an index of suspicion for this condition when patients describe continuous symptoms, especially long-term. Our case demonstrates the importance of MRI imaging and referral for specialist opinion, when persistent symptoms do not respond to conservative treatment as expected.
CONCLUSION
Although less common than in other joints of the synovium, osteochondromatosis can be found in the shoulder at the level of the joint recesses (including the sheath of the biceps long head tendon) and subacromial-deltoid bursa. The diagnosis can be made only on its characteristic features which, depending on the stage of the disease, may correspond to synovial proliferation, cartilaginous nodules (chondromas), and calcified or ossified nodules (osteochondromas).
REFERENCES
1.
Llaugher J, Palmer J, Rosón N, Bagué S, Camins A, Cremades R. Nonseptic monoarthritis: Imaging features with clinical and histopathologic correlation. Radiographics 2000;20 Suppl 1:S263–78. [CrossRef]
[Pubmed]

2.
Imhoff A, Schreiber A. Synovial chondromatosis. [Article in German]. Orthopade 1988;17(2):233–44.
[Pubmed]

3.
Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics 2007;27(5):1465–88. [CrossRef]
[Pubmed]

4.
Milgram JW. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg Am 1977;59(6):792–801.
[Pubmed]

5.
6.
Milgram JW. The classification of loose bodies in human joints. Clin Orthop Relat Res 1977;(124):282–9.
[Pubmed]

7.
Buess E, Friedrich B. Synovial chondromatosis of the glenohumeral joint: A rare condition. Arch Orthop Trauma Surg 2001;121(1–2):109–11. [CrossRef]
[Pubmed]

8.
Saotome K, Tamai K, Koguchi Y, Sakai H, Yamaguchi T. Growth potential of loose bodies: An immunohistochemical examination of primary and secondary synovial osteochondromatosis. J Orthop Res 1999;17(1):73–9. [CrossRef]
[Pubmed]

9.
Lunn JV, Castellanos-Rosas J, Walch G. Arthroscopic synovectomy, removal of loose bodies and selective biceps tenodesis for synovial chondromatosis of the shoulder. J Bone Joint Surg Br 2007;89(10):1329–35. [CrossRef]
[Pubmed]

10.
Walker EA, Murphey MD, Fetsch JF. Imaging characteristics of tenosynovial and bursal chondromatosis. Skeletal Radiol 2011;40(3):317–25. [CrossRef]
[Pubmed]

11.
Chen A, Wong LY, Sheu CY, Chen BF. Distinguishing multiple rice body formation in chronic subacromial-subdeltoid bursitis from synovial chondromatosis. Skeletal Radiol 2002;31(2):119–21. [CrossRef]
[Pubmed]

12.
Mohana-Borges AVR, Chung CB, Resnick D. Monoarticular arthritis. Radiol Clin North Am 2004;42(1):135–49. [CrossRef]
[Pubmed]

13.
Sheldon PJ, Forrester DM, Learch TJ. Imaging of intraarticular masses. Radiographics 2005;25(1):105–19. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Arthur Semedo Insumbo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Wilson Bizimana - Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FL Jroundi - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FZ Laamrani - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Arthur Semedo Insumbo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.