|
Case Report
Neuro-Behçet’s disease revealed by diencephalo-mesencephalic impairment
1 Radiologist Doctor, Firdaous Radiology Center, Kenitra, Morocco
Address correspondence to:
Jamal Aouifi
Firdaous Radiology Center, 84, Youssef Ibn Tachfine Avenue, 14000 Kenitra,
Morocco
Message to Corresponding Author
Article ID: 100021R02JA2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Aouifi J, Bouchama H, Eljouadi H, Hanine A. Neuro-Behçet’s disease revealed by diencephalo-mesencephalic impairment. Edorium J Radiol 2022;8(2):1–4.ABSTRACT
Introduction: Behçet’s disease is a systemic variable vessel vasculitis with unknown cause. Neurologic involvement known as neuro-Behcet’s disease (NBD) is often diagnosed in patients who present neurological symptoms and radiological lesions of the central nervous system.
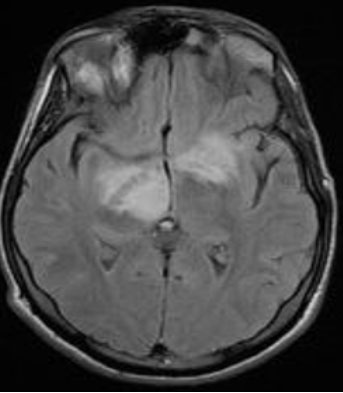
Case Report: A 42-year-old woman with a history of orogenital ulceration presented with behavioral disorders and heaviness of left hemibody. Brain magnetic resonance imaging (MRI) was performed and showed a pseudo-tumor diencephalo-mesencephalic area with T2 and Flair hypersignal, a slight hypersignal in diffusion sequence, and no contrast uptake.
Conclusion: Pseudotumoral NBD is a rare but severe manifestation of Behçet’s disease. Cerebral MRI is the most efficient method to explore, detect, and monitor parenchymal lesions.
Keywords: Brain MRI, Cerebral pseudo-tumor, Neuro-Behçet
INTRODUCTION
Behçet’s disease is a systemic variable vessel vasculitis with unknown cause whose main symptoms include skin-mucosa lesions and recurrent oral and genital ulceration [1].
Neurologic involvement known as Neuro-Behcet’s disease (NBD) is uncommon with a highly variable prevalence (5–59%) [1],[2]. It is often diagnosed in patients with known Behçet’s disease who present neurological symptoms and radiological lesions of the central nervous system. We present herein a case of pseudotumoral form of NBD.
CASE REPORT
A 42-year-old woman with a history of orogenital ulceration presented with behavioral disorders and heaviness of left hemibody, and headache. Physical exam showed pyramidal syndrome with left hemiparesis.
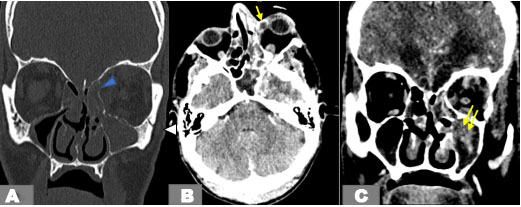
Brain MRI was performed in flair (Figure 1), diffusion (Figure 2), T1, T1 injected sequences (Figure 3), T2 (Figure 4), Gradient Echo, and 3D TOF T1, showing a diencephalo-mesencephalic lesion with hypersignal in T2 and flair, slight hypersignal in diffusion sequence and no contrast uptake. No venous thrombosis or arterial abnormality was detected.
DISCUSSION
Behçet’s disease is a systemic vasculitis whose neurological involvement, sometimes severe, is found in approximately 15% of cases [1],[2]. Neuro-Behçet’s disease pseudotumoral involvement has its own clinical characteristics: pyramidal signs and hemiparesis seem more frequent than in classic parenchymal forms [3].
The most common and most suggestive brain lesion is diencephalo-mesencephalic involvement, which is found half the time, followed by bulboprotuberant involvement in 40% of cases [4]. This lesional topography reflects a vasculitis affecting the small vessels predominating in the venous compartment. Mesencephalo-diencephalic lesions are often bilateral and asymmetrical, with contrast uptake in the initial phase [4],[5]. The differential diagnoses being mainly tumoral (glioblastomas or lymphomas) or infectious (tuberculous abscess) [5],[6].
In the context of brainstem involvement, cervical cord involvement by contiguity can be observed. Conversely, isolated myelitis is rarer, mainly seen as extensive lesions in height. It is most frequently a multifocal transverse myelitis, located in the cervical and dorsal regions, and which can be a factor of poor prognosis [7],[8].
The useful imaging examinations for the diagnosis of neuro-Behçet are head computed tomography (CT) with injection, and angio-MRI, with morphological sequences: T1, T2, gradient echo, diffusion sequences with ADC mapping [9],[10],[11],[12].
The lesions are asymmetrical and mainly distributed in the meso-diencephalic junction (46%), the pontobulbar (40%), hypo-thalamo-thalamic (23%), and the central gray nuclei (18.5%). The telencephalon is more rarely affected (7.7%) as well as the marrow (4.6%) [11],[12]. Several areas can be affected in the same patient. It should be noted, however, that the imaging may be normal in approximately 10–20% of cases, particularly in the acute forms, where the abnormalities may appear secondarily to the MRI [13]. Conversely, pathological imaging with neurologically asymptomatic Behçet disease is known as subclinical neuro-Behçet.
The lesions are hypointense in T1 sequence and hyperintense in T2 sequence, with an edematous area around the wound. In the acute phase, they take on contrast, with typical characteristics of inflammatory damage [9],[10],[11],[12],[13],[14].
The predilection for meso-diencephalic involvement could be explained by the venous anatomy. Indeed, telencephalic venous drainage occurs in two directions, through the existence of multiple anastomoses between the superficial, pial veins, and the basilar vein of Rosenthal. In the brainstem, these anastomoses are rarer [6],[9],[10].
In the pseudotumor forms, the lesions appear in hyposignal in T1 and in hypersignal in T2 with significant vasogenic edema and peripheral contrast uptake after injection of gadolinium [6],[15].
Di and telencephalic lesions are most often located in the white matter, deep or subcortical. They appear in T2 hypersignal and do not enhance. There are very few lesions of periventricular white matter, unlike demyelinating pathologies such as multiple sclerosis [15],[16].
CONCLUSION
Pseudotumoral NBD is a rare but severe manifestation of Behçet’s disease. It should be brought up in front of cerebral mass as a differential diagnosis. Cerebral MRI is the most efficient method to explore, detect, and monitor parenchymal lesions of the neuro-Behçet and that of the vessels.
REFERENCES
1.
Alfedaghi AS, Masters Y, Mourou M, Eshak O. A brain mass in a patient with Behcet’s disease: A case report. J Med Case Rep 2015;9:209. [CrossRef]
[Pubmed]

2.
Kontzialis M, Guryildirim M. Acute/subacute neuro-Behçet’s disease. Acta Neurol Belg 2017;117(4):925–6. [CrossRef]
[Pubmed]

3.
Yazici H. Behçet’s syndrome: An update. Curr Rheumatol Rep 2003;5(3):195–9. [CrossRef]
[Pubmed]

4.
Serdaroğlu P. Behçet’s disease and the nervous system. J Neurol 1998;245(4):197–205. [CrossRef]
[Pubmed]

5.
Uygunoğlu U, Siva A. Behçet’s syndrome and nervous system involvement. Curr Neurol Neurosci Rep 2018;18(7):35. [CrossRef]
[Pubmed]

6.
Mousa A, Okasha M, Isaacs J, et al. Brain pseudotumour secondary to Behçet’s disease. Ann R Coll Surg Engl 2019;101(8):e164–8. [CrossRef]
[Pubmed]

7.
Duprat JP, Ewert W, Muccioli C. Neuro-Behçet. [Article in Portuguese]. Rev Assoc Med Bras (1992) 2003;49(2):132. [CrossRef]
[Pubmed]

8.
Noel N, Drier A, Wechsler B, et al. Neurological manifestations of Behçet’s disease. [Article in French]. Rev Med Interne 2014;35(2):112–20. [CrossRef]
[Pubmed]

9.
Lee SH, Yoon PH, Park SJ, Kim DI. MRI findings in neuro-Behçet’s disease. Clin Radiol 2001;56(6):485–94. [CrossRef]
[Pubmed]

10.
Mnif N, Rajhi H, Mlika N, Kechaou S, Abdallah Nejmeddine B, Hamza R. MRI findings in neuro-Behcet’s disease. [Article in French]. J Neuroradiol 2006;33(4):250–4. [CrossRef]
[Pubmed]

11.
Borhani Haghighi A, Sarhadi S, Farahangiz S. MRI findings of neuro-Behcet’s disease. Clin Rheumatol 2011;30(6):765–70. [CrossRef]
[Pubmed]

12.
Shimazaki R, Sugaya K. Difference between the MRI findings for neuro-Behçet disease and neuro-sweet disease. Intern Med 2022. [CrossRef]
[Pubmed]

13.
Tali ET, Atilla S, Keskin T, Simonson T, Işik S, Yuh WT. MRI in neuro-Behçet’s disease. Neuroradiology 1997;39(1):2–6. [CrossRef]
[Pubmed]

14.
Yildiz S, Boyaci N, Sen Dokumaci D, Boyaci A. Different diffusion-weighted MRI findings in brainstem neuro-Behçet’s disease. BMJ Case Rep 2013;2013:bcr2013200738. [CrossRef]
[Pubmed]

15.
Oktay K, Guzel E, Yildirim DC, Aliyev A, Sari I, Guzel A. Primary pituitary abscess mimicking meningitis in a pediatric patient. Childs Nerv Syst 2021;37(10):3241–4. [CrossRef]
[Pubmed]

16.
Ben Taarit C, Turki S, Ben Maïz H. Pseudotumoral neurobehçet: A case report. [Article in French]. J Mal Vasc 2002;27(2):93–5.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jamal Aouifi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Houda Bouchama - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hajar Eljouadi - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ahmed Hanine - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Jamal Aouifi et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.